The footprint of a synthetic mesh in the pelvis: a report on experience with 48 cases
As an introductory to this session I would like to present a videoclip of the procedure needed to remove the Anterior portion of the Total Prolift System.
">
Anatomical Outcomes and Complications of the Total Vaginal Mesh (Prolift) Procedure for Pelvic Organ Prolapse
Synthetic mesh kits are wide employed in both the Netherlands and elsewhere, with a high incidence of Industry involvement- the main driving force is based unfortunately more on financial than proven medical safety and effectiveness. Re-operation rates is reported to be between 8, 5% (Diwadkar GB, et al, Obstet Gynecol. 2009; 113(2.1): 367-73) and 25% (Chris Mayer- abstract at IUGA 2009, Como).
In this report the experience of a peripheral gynaecologist is shared with the use of a polypropylene mesh kit, the Total Prolift System. It is an overview of experience gained in a rural hospital practise in the Netherlands- rural in the Netherlands means that the hospital is 120 km from the nearest Dutch teaching hospital. All the surgeries were done by the same surgeon (AJ Nieuwoudt) who had 26 years of experience in vaginal surgery. Training in the Prolift System was provided by Prof Jacquetin in Clermont-Ferrand. The surgical protocol followed in all cases was as laid down by Gynecare. A strict surgical auditing was prospectively followed, with interval communications with both the Dutch Pelvic floor workgroup and Gynecare. There was no financial involvement from industry.
The anatomical outcome with the placing- and assessment of complications experienced- of the Total Prolift System as first surgical choice in 48 consecutive patients with pelvic organ prolapse is reported. These procedures were done from the 1st of April 2005 to the 31st of January 2007, when the procedure was abolished for reasons that will become apparent.
The mean age of the patient population studied was 63yrs, with a variation between 31 and 78 yrs- only 5 cases were younger than 50yrs. 17 of the patients were sexually active. All patients had POPQ staging of the prolapse before surgery: 53% had at least stage 2 prolapse, and 47% stage 3 or more. 8 patients had previous prolapse surgery, with 2 incontinence surgery. 13 had a prior hysterectomy.
In the anterior compartment 90% had stage 2 prolapse (Aa=+2 – variation: -3 to +3 - Ba= +1.41 – variation: -3 to +6 – and C=-2). In the posterior compartment 90% also had stage 2 (Aa= 0 and Bp=+0.41). In the apical compartment 41% had stage 2, with 20% stage 3 – the mean for point C was +0,2.
The only noteworthy intra-operative complication was a ureter ligated with a haemostatic stitch on the bladder wall. The resultant ureter obstruction was diagnosed in the immediate post operative period. After vaginally removing the offending stitch in theatre, the obstruction was resolved- an IVP on 6 weeks confirmed no obstruction and no kidney damage. There were no bladder/or bowel intra-operative injuries.
2 cases of erosions were found on the 6 weeks assessment- one into the bladder- needing abdominal surgery- and one exposure (erosion through the suture line on the anterior vaginal wall). On 6 months 3 erosions presented- 2 on the posterior vaginal wall, and one on the anterior vaginal wall. The anterior vaginal wall erosion was in a sexually active patient and was away from the suture line scar. On 12 months a further 3 patients presented with erosions- all on the posterior wall on the perineum.
Follow-up of the patients were on 6 weeks, 6 months, 12 months, 24 months and 36 months
Patients were taken out of the study after a secondary procedure were done- this gives a 36 months availability for follow-up on 35 patients out of the initial 48. The secondary procedures will be alluded to later, but of note is that there is an accumulation of patients needing secondary surgery as time go by- after 36 months 25 out of 48 cases needed a form of secondary surgery, be it for poor results of prolapse repair or for correction of complications caused by the procedure.
Looking at results for the correction of prolapse, the poorest results were with apical support: on 6 weeks 8 cases had a bigger than grade 1 apical support failure (mean point C= -1, 68). One case had a posterior compartment prolapse greater than grade 2.
On 6 months symptomatic prolapse were present in 10% of cases (n=5). 10 cases had stage 2 or greater apical prolapse- representing 22% of cases operated on (C varied from -8 to +4). At this early stage 5 cases needed secondary surgery for apical prolapse (3 vaginal hysterectomies and 2 vault suspensions).
At 12 months 15% had in the anterior compartment a greater than stage 1 prolapse. 11 cases (33%) had an apical compartment prolapse, necessitating 5 vaginal hysterectomies and 9 vault suspensions. A further 4 (17%) had an apical prolapse on 24 months follow-up, necessitating in 2 cases vaginal hysterectomies and 3 vault suspensions.
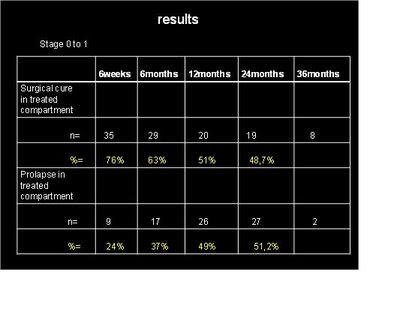
If successful surgery for prolapse is defined as being a leading edge stage 0 or less than stage 1, the following results emerged:
The tendency was an ever increasing prolapse in the treated compartment, ending with only 48,7% having successful surgical cure after 24 months.
Looking at which compartment that did the worse, it is obvious that the apical compartment is the offending compartment in nearly all cases with stage 2 or greater prolapse:
Focusing on secondary procedures needed, a clear picture comes to the fore: after 12 months 5 out of 39 cases were done, which increased to a total of 13 out of 36 (24 months) and 25 out of 35 (after 36 months).
The specific procedures are listed- note that after 36 months a total of 12 out of a possible 35 patients with uteruses needed a secondary hysterectomy to treat the apical prolapse. In 11 cases the anterior mesh were removed, necessitating a total re-do of the anterior wall support. These cases all had shrinkage of the anterior mesh, resulting in pain, either spontaneous or with intercourse:
Looking at the mean time interval between primary and secondary surgery, it became apparent that there is a delay of more than a year in most procedures. Even the two cases which needed a TVT-O due to de novo stress incontinence needed it after 25 and 30 months.
According to the Dindo classification of surgical complications, secondary surgery can be seen as a grade 3b complication: in 25 out of 48 studied a grade 3b complication was noted.
A special category of complication was noted, namely mesh shrinkage.Defining shrinkage as shortening of more than 50% of the distal to proximal distance, after 6 months 45 out of 46 the anterior portion of the Total Prolift System fullfilled the criterium. If one focus only on those that showed pain, whether spontaneous or with intercourse, 16 were present after 24 months- of these 14 required removal of the mesh. This was an acumilating effect.
Conclusion:
A few conclusions can be drawn from this study:
- In the author’s experience with 48 cases, poor anatomical outcomes were found with the use of the Total Prolift System in treating pelvic organ prolapse. This is especially true where the apical support is concerned.
- Significant complications were encountered; especially long term complications were a worrying feature. These needed a high incidence of secondary corrective surgery. The delayed feature of the onset of complications predict that the real incidence of complications is still to be seen.
- Shrinkage- also a delayed feature- of specially the anterior mesh is a serious complication. The only successful treatment there-of is removal of the mesh and a re-do of the prolapse surgery. This has a significant influence,not only on the morbidity, but also on the quality of live.
The use of synthetic meshes, especially in the anterior compartment, but also as a means of support to the apical aspect of the vagina cannot be supported.
The above had been presented by Andri Nieuwoudt at the 34 th Annual meeting of the International Uro-Gynaecology Assosiation on the 18th of June 2009 in Como , Italy.
Labels: polypropylene, prolift, synthetic mesh